
Case studies bring out the essence of clinical management. They represent true case scenarios and how they were handled in real-time. Patient confidentiality has been maintained throughout. The following case files are a glimpse into the possible offerings of genetics in modern medicine
 (Dr Shruti Bajaj: maiden name: Dr Shruti Agarwal)
(Dr Shruti Bajaj: maiden name: Dr Shruti Agarwal)
An 18-month-old female child presented to us with clinical features suggestive of nephrotic syndrome. Her physical examination and detailed family history highlighted the familial occurrence of abnormal nails, suggesting a diagnosis of the Nail-Patella syndrome. Nail-Patella syndrome is a rare cause of nephrotic syndrome in children. This case highlights the importance of a detailed history, including pedigree and a thorough examination of the patient.
 Our patient presented with congenital heart disease (Tetralogy of Fallot), hypocalcemia, hypoparathyroidism, and facial dysmorphisms. Suspecting DiGeorge syndrome (DGS), a fluorescence in situ hybridization (FISH) analysis for 22q11.2 deletion was made. The child had a hemizygous deletion in the 22q11.2 region, diagnostic of DGS. Unfortunately, the patient succumbed to the heart disease. DGS is the most common microdeletion syndrome, and probably underrecognized due to the varied manifestations. This case stresses the importance of a detailed physical examination and a high index of suspicion for diagnosing this genetic condition. Timely diagnosis can help manage and monitor these patients better and also offer prenatal diagnosis in the next pregnancy.
Our patient presented with congenital heart disease (Tetralogy of Fallot), hypocalcemia, hypoparathyroidism, and facial dysmorphisms. Suspecting DiGeorge syndrome (DGS), a fluorescence in situ hybridization (FISH) analysis for 22q11.2 deletion was made. The child had a hemizygous deletion in the 22q11.2 region, diagnostic of DGS. Unfortunately, the patient succumbed to the heart disease. DGS is the most common microdeletion syndrome, and probably underrecognized due to the varied manifestations. This case stresses the importance of a detailed physical examination and a high index of suspicion for diagnosing this genetic condition. Timely diagnosis can help manage and monitor these patients better and also offer prenatal diagnosis in the next pregnancy.
 (This child was initially seen at King Edward Memorial Hospital, Mumbai. The diagnosis was established while Dr Bajaj was attached to the Genetic Clinic KEMH, Mumbai as an Asst Professor )
(This child was initially seen at King Edward Memorial Hospital, Mumbai. The diagnosis was established while Dr Bajaj was attached to the Genetic Clinic KEMH, Mumbai as an Asst Professor )
A 4.5 year old female child, the only issue of her parents, was referred by an orthopedician in Ahmedabad, Gujarat. The child had approached the orthopedician for recurrent shoulder joint dislocations and buckling of the knee joints while running. Detailed history revealed that the child had looseness of the body since birth and delayed motor milestones. Detailed neurological work-up elsewhere considered the differential of a congenital muscle disorder. Clinical examination showed she had normal growth parameters, with joint and skin laxity and other tell-tale signs suspicious of a connective tissue disorder (rather than a primary muscle disease).
Advanced genetic test i.e. next generation sequencing (clinical exome), revealed that the child had a rare genetic condition, Ehler Danlos type 6. The couple was explained that this is a genetic disorder and that their next child has a 25% risk of having the same disease. The parents were explained the importance of regular follow up of the child for monitoring of known complications and for prenatal diagnosis in the next pregnancy. Proving the diagnosis not just ended a long diagnostic journey of the family; but also avoided the unnecessary muscle biopsy in the child.
The couple followed up some years later when the wife was pregnant again. Successful prenatal counseling was offered to the couple. The fetal cells of the next baby were checked for the same causative mutation (genetic error), seen in the case of the first child (having Ehler Danlos type 6). The expected baby in the womb did not have the causative mutation; assuring the couple that their second baby will not have the given genetic condition. The first child is under close follow-up for known cardiac and ophthalmological complications of Ehler Danlos Syndrome type 6. With active surveillance, we hope to nip any clinical problem in the bud and improve the quality of life of the child.
 A four day old male newborn was referred from a tertiary care NICU centre in Mumbai. The baby was born to a young couple who were related to each other by blood (first cousins). The child was born through normal vaginal delivery and weighed 3 kilograms at birth. After an initial uneventful period of two days, the baby suddenly had decreased feeding on the third day of life. This was followed by seizures and altered sensorium. He was comatose and unresponsive since the fourth day of life; necessitating mechanical ventilation and high-level intensive unit care. Inspite of the best medical care, the child succumbed on the fifth day. There was a significant family history. This couple had lost two previous children in an eerily similar fashion. Sensing that there could be a genetic basis to the given recurring disease, the physician had sought timely genetic opinion in this last baby’s case. A detailed and accurate pedigree analysis was outlined. An inborn error of metabolism was suspected. Also, special genetic tests were routed in time, not losing the precious window of opportunity to test the child.
A four day old male newborn was referred from a tertiary care NICU centre in Mumbai. The baby was born to a young couple who were related to each other by blood (first cousins). The child was born through normal vaginal delivery and weighed 3 kilograms at birth. After an initial uneventful period of two days, the baby suddenly had decreased feeding on the third day of life. This was followed by seizures and altered sensorium. He was comatose and unresponsive since the fourth day of life; necessitating mechanical ventilation and high-level intensive unit care. Inspite of the best medical care, the child succumbed on the fifth day. There was a significant family history. This couple had lost two previous children in an eerily similar fashion. Sensing that there could be a genetic basis to the given recurring disease, the physician had sought timely genetic opinion in this last baby’s case. A detailed and accurate pedigree analysis was outlined. An inborn error of metabolism was suspected. Also, special genetic tests were routed in time, not losing the precious window of opportunity to test the child.
The initial biochemical tests also pointed towards an inborn error of metabolism; proximal urea cycle defect or a mitochondriopathy. However, a biochemical diagnosis is not sufficient to prevent recurrence of the disease in the next child. For prevention of recurrence, one needs to know the error ‘at the level of the gene’ (i.e the mutation).
The child’s DNA was analysed after its death, by highly sophisticated technology, next-generation sequencing. This picked up the causative DNA error (mutation) which had resulted in three newborn deaths in the family. The mystery was unveiled; the cause was a genetic disease, a urea cycle defect. This disorder occurs, when each parent has one healthy copy of a gene and the other copy is a disease-causing one. When present in a single dose, the genetic error is insufficient to cause the disease, thus the parents remain asymptomatic throughout life. However, if the child inherits a disease-causing copy each from both the parents (homozygozity), it leaves no normal gene at the given position in the child. This precipitates the disease in such a child. However, by permutation and combination it is likely that the child may inherit both the healthy copies form both the parents or just one disease-causing gene, and the other one being healthy. In the latter two scenarios the child will remain asymptomatic. Having clinched the diagnosis at the level of the gene, it was possible to inform the couple an accurate risk of recurrence of the same disease in every subsequent pregnancy (25%).
With the genetic error outlined in this family, the couple was informed, that in the next pregnancy, they can select the embryos which do not have the given genetic mutation (preimplantation genetic diagnosis) and ensure the birth of an unaffected child. However, since this technology is relatively expensive, the couple was also counselled about the other option of prenatal diagnosis. In this method, when the mother is around 11-13 weeks pregnant, a small quantity of the fetal DNA is procured through a safe procedure (chorion villous biopsy). This fetal DNA can be checked for the disease-causing mutation in double dose (homozygozity). If present it predicts the same outcome as the previous pregnancies, in this baby too once it is born. In such a case, the parents can opt to discontinue the pregnancy medically and legally, before 20 weeks of pregnancy. On the other hand, if the baby inside is normal or carries just one copy of the disease-causing mutation, then the parents can continue with the pregnancy without stress and anxiety.
 A young couple presented to us, prior to planning their next pregnancy. They had an older four-year old male child, diagnosed with autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD). The child also had history of seizures and disturbed sleep. The couple was concerned about the risk of recurrence of similar symptoms in the next baby. Clinical assessment of the child by the Geneticist revealed him to have tall stature, central hypotonia, relative macrocephaly and non-specific facial dysmorphisms. The family history was unremarkable.
A young couple presented to us, prior to planning their next pregnancy. They had an older four-year old male child, diagnosed with autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD). The child also had history of seizures and disturbed sleep. The couple was concerned about the risk of recurrence of similar symptoms in the next baby. Clinical assessment of the child by the Geneticist revealed him to have tall stature, central hypotonia, relative macrocephaly and non-specific facial dysmorphisms. The family history was unremarkable.
The couple was explained that one can reliably help predict the risk of recurrence in the future pregnancies, ONLY IF we can establish a precise genetic cause of ASD in the older child (index patient). The couple was explained that ASD can have genetic and non-genetic causative factors. Within, the genetic landscape, causative errors could be within single genes (monogenic) or multiple genes (polygenic). Current testing platforms can reliably detect only monogenic errors. Thus, they were explained these tests may not necessarily always be helpful in establishing the cause of ASD in every child. As per literature, the yield of genetic tests in ASD ranges from 10% to 40%.
Review of old records showed normal blood TMS and urine GCMS, basic laboratory parameters (CBC, TFT, B12, CPK) and MRI brain. His EEG was abnormal.
After thorough pre-test genetic counseling by our Clinical Geneticist, first tier genetic tests were ordered. These included Karyotype, Chromosomal microarray 750K (CMA750K) and TPPCR for Fragile X. These tests results returned normal.
The couple was counseled that normal results do not necessarily mean an absence of genetic causation. The empiric risk of recurrence in the next pregnancy was slated to be between 15-20%, based on various literature sources.
The couple opted for tier two test- viz, Whole Exome sequencing (WES), after a robust pretest counseling session. They were explained that WES can sometimes yield uncertain and unactionable genetic findings. Possibility of inconclusive results on WES was also reiterated.
However, the results of WES were rewarding. It revealed a likely pathogenic variant (also called as mutation) in CHD8 gene, associated with Intellectual developmental disorder with autism and macrocephaly (IDDAM). Parental test by Sanger for the same CHD8 gene variant revealed the variant to occur de novo (i.e ‘on its own’) in the child. Thus, the CHD8 mutation was not inherited from the parents, rather had occurred ‘naturally’. The clinical features of the child matched with the diagnosis suggested by the test.
Plan for the next pregnancy: Since this disorder occurs sporadically in nature, the risk of recurrence was barely 1-2% in the next pregnancy. The couple found this information very reassuring. To be doubly sure, they tested the fetal DNA in the next pregnancy via chorion villous biopsy at 11 weeks of gestation. The fetus was found to be unaffected. They continued the pregnancy to term and delivered a healthy child, who is normal at the 30-month follow up.
Conclusion: The case demonstrates the role of new-age genetic tests in providing closure to families having a child with autism. While the causes of autism can be multifactorial, the case enables us to appreciate the contribution of genetics to autism, and the rewards of detecting it in time. Timely diagnosis can help prevent recurrence of the same disease in the future pregnancies.
 A 40-yr old anesthesiologist, Dr Shanta (name changed) presented to us with family history of premenopausal breast cancer in her mother, claiming her mother’s life at the age of 40 years. Her mother’s sister had also succumbed to ovarian cancer at the age of 45-years. A three-generation pedigree elicitation by our qualified Clinical Geneticist revealed that Dr Shanta’s maternal grandfather also succumbed to prostate cancer.
A 40-yr old anesthesiologist, Dr Shanta (name changed) presented to us with family history of premenopausal breast cancer in her mother, claiming her mother’s life at the age of 40 years. Her mother’s sister had also succumbed to ovarian cancer at the age of 45-years. A three-generation pedigree elicitation by our qualified Clinical Geneticist revealed that Dr Shanta’s maternal grandfather also succumbed to prostate cancer.
Dr Shanta’s recent mammogram, CA125 and transvaginal USG (TVUSG) returned normal. She was concerned about the risk of her family cases being connected via a common genetic error. Based on the pedigree, the chances of her mother harboring a HBOC variant was one of the possibilities. Dr Shanta was understandably worried about the possibility of herself harboring a variant/ mutation in one of the Hereditary Breast and Ovarian Cancer (HBOC) predisposing genes too.
A detailed pre-test genetic counseling session was undertaken for the patient. Dr Shanta was explained that ideally the index patient’s DNA should be tested first. Once we detect the family-specific mutation in one of the HBOC genes in the affected patient, the same is then tested in other members desiring a pre-symptomatic screening. However, in her case, there were no living patients available for DNA testing.
Dr. Shanta was explained the strengths and limitations of the oncogenetic tests in an asymptomatic healthy individual. While they can prove to be very helpful in some cases, they can also occasionally be distressing due to ‘uncertain’ and ‘unclear’ results. The ‘cancer phobia’ may only get worsened with such unclear findings; she was carefully explained. She was also explained that a failure to detect a pathogenic variant in a healthy individual, does not eliminate the possibility of a HBOC predisposing pathogenic variant being present in the family. Around 10-18% of the Indian patients with suspected BRCA1/ BRCA2 variants may not be detected on the routine first tier ‘oncogenetic test’ (exome sequencing panel tests) and this may necessitate a second-tier test (i.e MLPA for BRCA1 and BRCA2) After understanding all aspects of genetic testing in discussion with our Geneticist, she opted for the oncogenetic panel by exome sequencing.
The test revealed Dr Shanta to carry a pathogenic variant in the BRCA1 gene, which indicated that she was predisposed to breast and ovarian cancer. The post-test genetic counseling session stressed on the penetrance of the variant, the chances of her developing the associated cancers, the risk-reduction modalities available and the role of cascade testing in the as-yet asymptomatic relatives >18 years of age.
She was referred to an oncologist as well as an oncosurgeon. She was explained the importance of regular onco-surveillance. Risk reduction modalities (surgical versus chemoprevention) were discussed with her. Her annual mammograms, breast MRI, CA125 and TVUSG have been returning normal for the last 2 years. Since her family is complete with two kids, she has been contemplating upon the role of bilateral mastectomy and removal of her uterus, bilateral ovaries and fallopian tubes; in due discussion with the oncologist.
Conclusion: The case highlights the strength of modern age genetics in preventive oncology.
 A 6-month infant child, hailing from rural Maharashtra, presented to us with seizures since the last two months. His antenatal and perinatal period was uneventful. The child was normal until 4 months of age when the first seizure appeared. His MRI brain, EEG, serum B12 level done elsewhere, were normal. The child’s seizures were partially responsive to the ongoing anti-seizure medications. Developmentally, he had mild motor delay too.
A 6-month infant child, hailing from rural Maharashtra, presented to us with seizures since the last two months. His antenatal and perinatal period was uneventful. The child was normal until 4 months of age when the first seizure appeared. His MRI brain, EEG, serum B12 level done elsewhere, were normal. The child’s seizures were partially responsive to the ongoing anti-seizure medications. Developmentally, he had mild motor delay too.
Our Geneticist evaluated the family in detail. It revealed the child to have cutaneous rash as well as alopecia and oral candidiasis. These simple sings served as very important clues to the possibility of an underlying biotinidase deficiency. Biotinidase deficiency is an inherited genetic disorder that occurs due to a metabolic defect in recycling vitamin biotin. This condition, can be easily treated with 5-10 mg of daily oral biotin, an easily available and cheap drug. Individuals with this disorder can present in early childhood with seizures, deleted development, gait difficulties, vision and hearing loss. Individuals with this condition may also exhibit lack of scalp hair (alopecia). Once vision problems, hearing loss, and developmental delay occur, they are usually irreversible, even with biotin therapy. Some individuals with this condition may present first even in adulthood.
A simple blood test revealed deficient serum biotinidase level in the child. Thus, a diagnosis of biotinidase deficiency was established in the child. His hearing and vision were tested to be normal.
The child was started on 10mg daily oral biotin, to be continued lifelong. The monthly expense of this drug was less than 400 INR per month. The child’s seizures abated with oral biotin. The other antiepileptic medications were gradually tapered and stopped over the years to come. The family was counseled to ensure thorough compliance with the biotin therapy.
Conclusion: A delay in the diagnosis can deprive the patient of the benefits of timely therapy, when available. Although, many genetic therapies and medications are expensive, this case serves as a reminder, that certain treatment options for some diseases may be very simple and inexpensive; provided these disorders are suspected in time.
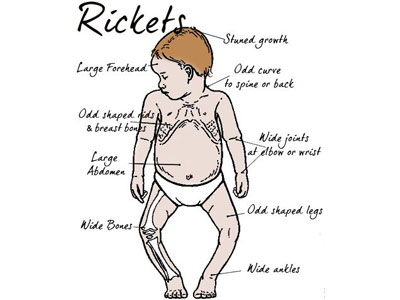 A 5-year-old boy presented with a tetanic spasm of the hands. Examination revealed short stature and bony deformities (knock knees, prominent wrists). He had history of one sibling death to hypocalcemia tetany and seizures.
A 5-year-old boy presented with a tetanic spasm of the hands. Examination revealed short stature and bony deformities (knock knees, prominent wrists). He had history of one sibling death to hypocalcemia tetany and seizures.
This child was misdiagnosed as Vit-D deficient rickets elsewhere and was being treated with 25(OH) Vit-D and oral calcium; with no benefit. His X rays showed cupping and fraying of metaphyseal ends of the radii, ulna and femurs; suggestive of rickets. The laboratory parameters (low serum calcium, normal phosphorus, elevated ALP and PTH, paradoxically elevated 25-OH VitD), however suggested the possibility of a close clinical cousin, viz, Vitamin-D ‘resistant’ ricket- type 1a (VDRR1a). Although externally the manifestations can be similar to rickets, it is a close analysis of the biochemical parameters and a lack of response to Vit D that helps one to suspect in this direction. Our suspicion was heightened by a low level of 1,25 (OH)2 Vit D, which in sync with elevated 25(OH) Vit D is a crucial hint pointing towards VDRR1a.
Genetic testing with clinical exome sequencing, prove our suspicion to be right, indeed!
The diagnosis of VDRR-1s (gene: CYP27B1) was rewarding since, changing the medicines from 25(OH) Vit D to 1,25(OH)2 Vit D formulation (Calcitriol), along with oral calcium carbonate, helped the child’s features resolve gradually over time. He has not had any episodes of tetany on follow up. His serum calcium has normalized. He also gained 3-centimeters height in 6 months.
Conclusion: The case highlights the role of a trained Geneticist in picking up the red flags for ‘genetic rickets’ early, and helping the family mitigate the complications associated, by instituting timely and correct therapy.
 A 25-year-old pregnant lady, carrying her first pregnancy, presented to us with an abnormal 18-week anomaly scan. The scan showed the child inside the womb (i.e fetus) to have severe hydrops (accumulation of fluid in various compartments of the body) including pericardial effusion. The fetus’s nuchal thickness was also grossly elevated (4mm) with documentation of internal septations. The couple did not have any family history of a similarly affected fetus; nor any significant history of any member with intellectual or physical disability. The treating obstetrician had ruled out common non-genetic causes of fetal hydrops.
A 25-year-old pregnant lady, carrying her first pregnancy, presented to us with an abnormal 18-week anomaly scan. The scan showed the child inside the womb (i.e fetus) to have severe hydrops (accumulation of fluid in various compartments of the body) including pericardial effusion. The fetus’s nuchal thickness was also grossly elevated (4mm) with documentation of internal septations. The couple did not have any family history of a similarly affected fetus; nor any significant history of any member with intellectual or physical disability. The treating obstetrician had ruled out common non-genetic causes of fetal hydrops.
Fetal hydrops can be caused due to many reasons. Amongst these, it is noteworthy, that known genetic causes contribute to nearly 25-30% of all cases of fetal hydrops; a likely underestimate. Amongst the genetic causes some of them include: chromosomal deletions or duplications, Down syndrome, certain single gene errors including alpha thalassemia, inborn errors of metabolism, lysosomal storage diseases etc. Some of the genetic errors occur for the first time in the fetus (sporadically/ naturally occurring); whilst some occur due to ‘inheritance’ of the damaging mutations from the parents.
Repeat scan done at 19 weeks showed the same findings, with some worsening of the hydrops. The chances of postnatal survival and normal neurological outcome was predicted to be very guarded and poor in this case. Our Geneticist helped the couple to obtain complete information about the likely prognosis and causative factors of fetal hydrops in their baby. Genetic counseling was offered in a ‘non-directive’ and a ‘non-biased’ manner. The final decision to continue the pregnancy, versus, terminating the same was rested upon the couple.
Due to the poor prognosis associated, the couple decided to terminate the pregnancy in line with the existing PCPNDT laws in India.
They were counseled that if the fetal hydrops was secondary to a genetic factor that was inherited from either or both the parents, there existed a risk of recurrence (empirically, as high as 25%) for the same pathology in the future pregnancies too. The parents consented to get the fetus tested, with the hope of getting a closure and a diagnosis in this case. The terminated fetus was analyzed in detail. First tier genetic test (chromosomal microarray) returned normal. However, the next genetic test, whole exome sequencing, revealed the fetus to carry damaging mutations in both the copies of the gene resulting in mucolipidosis type 2. This is an autosomal recessive condition that occurs due to the inheritance of a faulty gene, one from each of the healthy parents. There existed a 25% risk of recurrence of the same disease in the future pregnancies.
The couple was made aware of the options available to them to prevent a recurrence in the future pregnancies, by a detailed reproductive genetic counseling. They opted for prenatal testing by chorion villous biopsy in the next pregnancy, at 11 weeks of gestation. The fetal DNA was tested and was found to carrying normal alleles of the gene responsible for mucolipidosis-type 2, in the previous child. Thus, the couple was reassured about the likelihood of this baby being normal. They continued the baby to term. This child is normal and growing well at the 2-yr follow up.
 A recently married couple in their late-30s, presented to us for preconception genetic counseling. They both had progressive vision loss. The husband reported the onset of symptoms in early childhood, with night blindness in the initial years of the complaints. The wife developed symptoms of night blindness in her late teens. She too had initial night blindness, progressing gradually to even day-time vision loss. They both had significant visual impairment at the time of presentation. They were normal intellectually. They denied any hearing concerns.
A recently married couple in their late-30s, presented to us for preconception genetic counseling. They both had progressive vision loss. The husband reported the onset of symptoms in early childhood, with night blindness in the initial years of the complaints. The wife developed symptoms of night blindness in her late teens. She too had initial night blindness, progressing gradually to even day-time vision loss. They both had significant visual impairment at the time of presentation. They were normal intellectually. They denied any hearing concerns.
Detailed history revealed that the husband had a similarly affected younger sister, while the wife had no other affected members. The husband’s parents were married consanguineously, while the wife’s parents were non-consanguineous.
Ophthalmic evaluation and ERG previously done, reported retinitis pigmentosa (RP) in both of them. The husband additionally had history of premature cataracts. He also had bilaterally, an extra finger on the ulnar side (post-axial polydactyly)
Retinitis pigmentosa is an inherited disorder of the eye. Some of the cases occur sporadically in nature, while some are due to inherited mutations from either/ both parents. There exist >3000 mutations, across the >70 known genes responsible for retinitis pigmentosa. Detecting the exact cause can help families take informed reproductive decisions.
The couple was keen to know the chances of them having a child with retinitis pigmentosa too. We offered whole exome sequencing to the couple. This test checks the coding parts (i.e exons) of nearly 22,000 genes in the human cell. Pretest genetic counseling highlighted on the prospects of negative, uncertain or inconclusive results. They were informed that they can be guided confidently in respect to their preconception query only if the test yielded definite and conclusive genetic results.
The test revealed the husband to be harboring homozygous pathogenic variants/ mutations (i.e both allele copies of a given gene affected) in the CFAP418 gene, indicating autosomal recessive, retinitis pigmentosa- type 64. The variants/ mutations in the husband were inherited, one from each of his parents. However, the parents had another normal functioning gene copy too, and thus were unaffected (i.e his parents were only CARRIERS for the given gene variation)
The wife fortunately had another genetic cause of RP. She was detected to harbor hetero pathogenic variant/ mutations (i.e both allele copies of a given gene affected) in the SLC7A14 gene, indicating autosomal recessive retinitis pigmentosa-type 68. The variants/ mutations in her were inherited, one from each of her parents. However, the parents had another normal functioning gene copy too, and thus were unaffected.
Thus, the couple was counseled that they had different causes of genetic blindness. The two genes responsible in this case have not been reported to cause ‘digenic RP’. Thus, in such scenarios, there is usually NO ADDED RISK OF RECURRENCE of blindness due to retinitis pigmentosa, as compared to the general population, in the prospective child. They were reassured and planned their prospective child after due routine preconception checking by their obstetrician.
 A 5-year-9-month-old girl came to us with chronic cough and poor growth. She was diagnosed in 2022 with Neurofibromatosis type 1 (NF1) — a genetic disorder that can cause benign nerve tumors (neurofibromas), skin pigmentation (café-au-lait spots), and sometimes learning or behavioral difficulties. Other organs such as the eyes, bones, lungs, and endocrine system can also be affected.
A 5-year-9-month-old girl came to us with chronic cough and poor growth. She was diagnosed in 2022 with Neurofibromatosis type 1 (NF1) — a genetic disorder that can cause benign nerve tumors (neurofibromas), skin pigmentation (café-au-lait spots), and sometimes learning or behavioral difficulties. Other organs such as the eyes, bones, lungs, and endocrine system can also be affected.
NF1 is relatively common, occurring in about 1 in 3,000 births, and in nearly half of the cases, the mutation in the NF1 gene arises spontaneously, with no family history.
Our patient had a large inoperable mediastinal plexiform neurofibroma — a tumor pressing on the trachea and lung. This caused breathing difficulty and feeding issues.
In 2020, the U.S. FDA approved Selumetinib, an oral targeted therapy for children with symptomatic, inoperable plexiform neurofibromas. The drug works by shrinking tumor size and improving quality of life.
Although Selumetinib was not available in India at the time of diagnosis, the family remained in regular follow-up. By 2024, her symptoms had worsened with dysphagia (difficulty swallowing), obstructive sleep apnea, and tumor progression. Through AstraZeneca’s patient-assistance program, the child began Selumetinib therapy in October 2024.
After six months of treatment, her MRI showed approximately 50% tumor reduction, along with marked improvement in breathing, swallowing, sleep, and growth, and no significant side effects.
Key Takeaway: This case demonstrates how timely diagnosis and genetic evaluation of NF1 can open the door to targeted therapy and significantly improve outcomes.
With the availability of Selumetinib in India, children with NF1 and inoperable plexiform neurofibromas now have access to an effective, evidence-based treatment option that can enhance both health and quality of life.
 A young, non-consanguineously married couple visited our clinic during their ongoing pregnancy after a routine ultrasound scan showed that their baby had isolated Binder facies — a condition where the middle part of the face (including the nose and upper jaw) appears underdeveloped, giving a flat facial profile.
A young, non-consanguineously married couple visited our clinic during their ongoing pregnancy after a routine ultrasound scan showed that their baby had isolated Binder facies — a condition where the middle part of the face (including the nose and upper jaw) appears underdeveloped, giving a flat facial profile.
Naturally, the finding caused significant concern for the expectant parents, who wanted to understand the cause and implications for their baby.
After detailed pre-test genetic counseling, the couple decided to proceed with amniocentesis—an invasive test where a small amount of amniotic fluid is drawn for genetic analysis. The fetal chromosomal microarray and whole exome sequencing were performed to look for any underlying genetic or chromosomal cause.
The test results did not reveal any definite genetic abnormality. A few variants of uncertain significance (VUS) were detected, but these were considered unlikely to explain the facial appearance. In line with international guidelines, the absence of other structural abnormalities and the isolated nature of Binder facies were discussed in detail with the couple.
Through non-directive counseling, we explained that when Binder facies appears in isolation, the prognosis is usually very favorable, with normal brain development and good long-term outcomes. The couple felt reassured and chose to continue the pregnancy.
A few months later, they welcomed a healthy, full-term baby, who continues to grow and develop normally.
Key Takeaway: Facial differences such as Binder facies (maxillonasal dysplasia) can understandably create anxiety for parents. However, when such features occur without other abnormalities, the outcome is often excellent.
A careful antenatal genetic approach—including detailed ultrasound review, appropriate genetic testing, and sensitive, evidence-based counseling—can help families make informed choices and avoid unnecessary interventions or termination of a healthy pregnancy


