Genetics of Breast Cancer
Mrs. Shalaka (name changed), 43-year old young professional, lost her mother to ovarian cancer. Her mom’s death was the proverbial ‘last straw’ on her worried back. Her pedigree revealed that her maternal aunt and grandmother had expired due to breast cancer in their early 50s. Shalaka didn’t take long to understand that she was at a high risk for hereditary breast and ovarian cancer (HBOC) too. Subsequent to detailed pre-test genetic counselling, she underwent an oncogenetic test which revealed that she was indeed a carrier for a harmful mutation in the BRCA1 gene, most likely inherited from her maternal lineage. She did carry a significant chance of developing breast and ovarian cancer. She was explained the various options to reduce the risk of developing ovarian and breast cancer, including certain oral medications and/or risk reduction surgeries to remove her breasts and ovaries. She opted for the latter. Morose though it may sound, bilateral removal of the breasts, ovaries along with the fallopian tubes is often tipped as the option that confers maximum risk reduction to patients carrying the BRCA gene mutation. Our memories serve us better, when there is a celebrity like Angelina Jolie endorsing the fact, who herself underwent the procedure in a staged manner, following the revelation of her BRCA1 positive status. “It’s relieving as well as empowering”, Shalaka quipped. She said, “My post-op bed was fanned by a 70-year old lady undergoing palliation for an advanced stage of terminally detected breast cancer, on one side; and another lady who lost her battle to ovarian cancer, due to late detection again, on the other side. Both of them had strong family histories. Makes me wonder, did they miss checking something early on? Do they have children? Wouldn’t their kids want to know if there was a mutation lurking in one of the ‘cancer-genes’?”
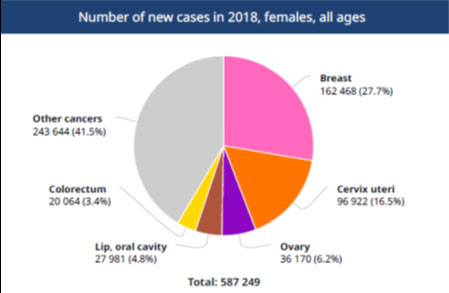
Breast cancer has been documented to be the commonest cancer, globally in 2018, as per World Health Organisation [Figure 1]. In the year 2018, over 1.5 lakh new cases and 87,090 deaths were reported due to breast cancer, in India alone. [1, 2] Nearly half of the breast cancers in India are usually detected late in stage 3 or 4, highlighting a delayed diagnosis and lack of awareness in the general population. [2]
Nearly 15-20% of breast cancer is due to an underlying genetic susceptibility and associated with familial clustering. Around 5-10% of the breast cancer cases are due to well-delineated genetic causes; called as hereditary breast and ovarian cancer (HBOC) syndromes. Although BRCA 1 and 2 genes are responsible for around 25% of the HBOC syndromes, these are not the only candidate genes to be suspected in hereditary cancer syndromes. [3] Some other familial cancer genes include TP53, ATM, BRIP1, CHD1, PALB2, RAD51C and RAD51. [3, 4] While pure genetics is not the commonest cause of breast cancer, it is very likely under-suspected, under-diagnosed and swept under the rug in formal discussions with patients regarding breast cancer.
Why should we diagnose HBOC syndromes? [4,5]
1. Implications for the patient- surgical: HBOC syndromes are associated with a 60-80% lifetime risk of developing breast cancer, 20-40% lifetime risk of ovarian cancer and low risk for developing other cancers like pancreatic, colon, uterine cancer and melanomas.
Unlike breast cancer, ovarian cancer known to be associated with HBOC, is not easily diagnosed ‘early’ on regular surveillance. Late presentation and metastasis in ovarian cancer are associated with higher mortality. Thus, if the patient is undergoing breast reduction surgery for breast cancer, and realises that she has the BRCA mutation, her surgical options may include an additional, often lifesaving, ovary and fallopian-tubes removal surgery too.
2. Implications for the patient- medical: A patient with breast or ovarian cancer due to BRCA1 mutation is known to respond better to certain drugs like PARP inhibitors and platinum agents, especially in recurrent disease.
These decisions are best taken in conjunction with an Oncosurgeon and Oncologist, who would be the main drivers for the rest of the holistic cancer management too.
3. Implications to the family: HBOC syndromes are known to follow autosomal dominant inheritance. In such cases, there is a 50% chance that the patient can pass the harmful mutation to the next generation. For example, if the lady has inherited the damaging ‘mutation’ from one of her parents, then it is likely that even her siblings and their progeny are at a risk of harbouring the same harmful mutation. Early and targeted genetic testing of the extended family members can give these ‘as-yet’ asymptomatic individuals an opportunity to understand their risks and mitigate the same by timely surveillance and risk reduction options, as appropriate. Simple measures like self-breast examination and annual mammography for the ‘high-risk’ family members, can also play an important role in early detection of breast cancers.
The aspect of ‘selective and preventive genetics’ to prevent cancer in the future generations through prenatal testing may be debatable for oncogenes like BRCA1/2, which manifest in adulthood. However, there are some cancer genes like TP53 which have implications in very aggressive childhood cancers. The latter would be a better-accepted candidate than BRCA1/2 for prenatal diagnostics (PND) and preimplantation genetic diagnosis (PGD) to avoid future affected generations; although such discussions need to be individualised and personalised, ultimately.
When to suspect a hereditary breast cancer syndrome? [3,4, 5]
Table 1 highlights the red flags in diagnosing the HBOC syndromes. [2, 3]
It is possible that the deleterious gene could have come from the paternal grandmother or paternal aunt, through an unsuspecting male (father/ brother). The males who carry BRCA mutation may be asymptomatic, but are also at an increased risk of breast, pancreatic and prostatic cancers. Thus, while taking a four-generation pedigree; it is imperative to not underestimate the cancer occurrences in the paternal as well as the maternal lineages.
Table 1: Red flags for suspecting genetic susceptibility to breast cancer
| Early onset breast cancer in the patient, especially if premenopausal or ≤ 45 years |
| Breast cancer at ≤ 50 years, with ≥1 first or second degree relatives with breast cancer or≥1 first or second degree relatives with ovarian cancer |
| Breast cancer with one or more of the following cancers on the same side of the family Sarcoma, Brain tumour, Thyroid cancer, Leukaemia, Lymphoma, Endometrial cancer, Pancreatic cancer, Gastric cancer |
| Ovarian cancer at ANY age |
| Family history of breast/ and or ovarian cancer |
| Family history of multiple affected members |
| Triple negative breast cancer diagnosed ≤ 60 years |
| Personal history of multiple primary cancers |
| Personal/ family history of male breast cancer |
| Two primary breast cancers in the same person |
What are the genetic tools that can help diagnose HBOC? [4,5]
With the advent of sophisticated diagnostic tools, it is possible to detect the germline mutations in the genes associated with HBOC. The test methodology most useful in this regard is Next generation sequencing (NGS), followed by Multiplex ligation probe dependent amplification (MLPA).
There are three possibilities when one runs an NGS panel for hereditary cancer syndromes:
Possibility 1: Test yields no result i.e. negative: One needs to appreciate that a negative genetic test doesn’t necessarily mean ruling out a HBOC. One may need to look at other genes not tested in the panel or choose another genetic tool in some cases.
Possibility 2: Test yields a pathogenic variant i.e positive. Implications need to be discussed with the Oncology and Genetic team.
Possibility 3: Test results are ambiguous [variant of uncertain significance (VOUS)]; a vast majority of which get reclassified as benign with time. [6] However, some VOUSs may actually get upgraded to being pathogenic, as further data about the mutation accumulates. The implications of a ‘reclassification’ on either side is very serious, and so close communication with a Genetic expert is recommended.
It is truly said- ‘Knowledge is the new RICH! Arm yourselves with it.’ October is the month of ‘Breast cancer awareness’. The above blog is an attempt to raise awareness about the role of genetics and genetic counselling along with detailed pedigree elicitation in suspected familial breast cancers and the strengths and flaws of the newer tests to detect the causative genetic errors in the same.
Figure 1a: Top cancer per country as per 2018 data: Global Cancer Observatory (World Health Organisation)
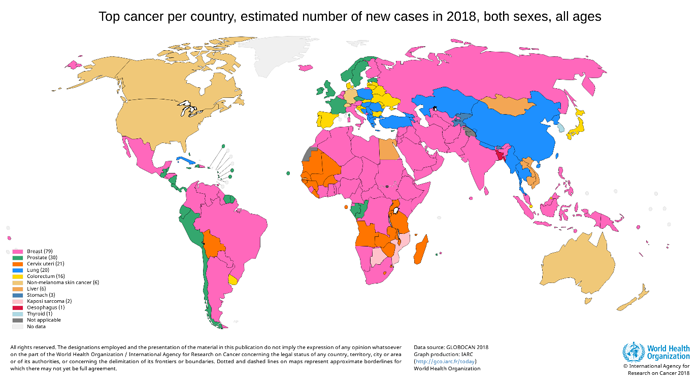
Figure 1b: Number of new cancer cases in females in India and its distribution (2018): Global Cancer Observatory. URL:https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf
References:
1.URL: https://gco.iarc.fr/today/online-analysis-map?v=2018&mode=cancer&mode_population=continents&population=900&populations=900&key=total&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=10&group_cancer=1&include_nmsc=1&include_nmsc_other=1&projection=natural-earth&color_palette=default&map_scale=quantile&map_nb_colors=5&continent=0&rotate=%255B10%252C0%255D (accessed on 24 Aug 2020)
2.URL: https://gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf (accessed on 24 Aug 2020)
3. Hereditary cancer syndromes. In: Practical Genetics for the Ob-Gyn. Editors; Hogge A, Rajkovic A. McGrawHill publications, China, 2015.
4. Hereditary breast and ovarian cancer syndromes. In: Handbook of cancer genetic counseling and risk management. Editor; Sarin R. Tata Memorial Hospital, India, 2018.
5. Petrucelli N, Daly MB, Pal T. BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer. 1998 Sep 4 [Updated 2016 Dec 15]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1247/
6. So MK, Jeong TD, Lim W, et al. Reinterpretation of BRCA1 and BRCA2 variants of uncertain significance in patients with hereditary breast/ovarian cancer using the ACMG/AMP 2015 guidelines. Breast Cancer. 2019;26(4):510-519. doi:10.1007/s12282-019-00951-w